The release of a report by the Australian National Centre in HIV Epidemiology and Clinical Research (NCHECR) in February this year contained arresting news for government HIV/AIDS organisations. The predictions through to 2015 for new HIV infection rates were an increase of 20 percent in Queensland and an alarming 73.5 percent in Victoria. But there was welcome news as well. Over the same period NSW was set for a 12 percent decrease in new HIV infections.

Australian Federation of AIDS Organisations executive director and co-chair of the Global Forum on MSM and HIV Don Baxter says given the criteria used the projections aren't surprising. "This mathematical projection uses behaviours up to mid 2007 and the preceding five years to predict future HIV infection rates. The two key differences between NSW and Victoria and Queensland are that NSW didn't reduce funding from 1996 on, and that in NSW HIV partnership works.
"The relationship between doctors, government departments and HIV/AIDS committees works well in NSW but this hasn't been the case in Victoria or Queensland over the past ten years. The Queensland government tendered out its HIV/AIDS services between 2004-2007 which caused a lot of suspicion between organisations. And it is unfortunate that the recent campaigns by the Victorian government fell outside the timeframe of this study, however the problem in Victoria remains that funding isn't ongoing."
NSW's enviably low HIV rates are due not only to government commitment says AIDS Council of NSW (ACON) CEO, Stevie Clayton. "Even though the NCHECR predictions are based primarily on condom use and rates of STI infection there are a range of factors to consider.
"When we compare the different states, particularly Queensland and Victoria, currently more, or a higher proportion of gay men in NSW are in monogamous relationships, there are fewer who report that they have casual partners, there are fewer who report that they have many casual partners. We are seeing a decrease in the number of people who are in serodiscordant relationships, where one is HIV positive and the other is HIV negative, or serononconcordant, where they don't know if they have the same sero status or not.
"We see slightly higher rates of testing, so more gay men know their HIV status and can make decisions around that, and we see slightly higher rates of disclosure. This means more men are talking about their HIV status when they are negotiating sex, so again that provides the opportunity to negotiate the sort of sex they might consider appropriate for a serodiscordant relationship.
"At ACON we think all of these factors have an impact on HIV infection but it's also about the nature and structure of community; the types of campaigns we do, where we focus our effort. We do HIV in a much broader health context. There are many more opportunities for us to engage with people about a health issue so we can slip in HIV prevention work which fits in better in the context of people's lives. There has also been a much greater investment by the NSW government in funding HIV prevention work with gay men for the last ten years."
This message is echoed by Baxter. "ACON has had more funds to do saturation campaigns, support programs and counseling, but it's success is also due to it's comprehensive program based on age, ethnicity, sero status and location, within Sydney and across the state."
Clayton says ACON focuses on the social determinants of health. "We know most gay men in NSW today know that condoms and lube will protect them from HIV and many STIs, and if they're not consistently using them it's because of other decisions they're making or other social factors, such as drug and alcohol use, homelessness and mental health problems.
"We know that about a third of new infections are those who are in long-term relationships, so we do a lot of work on relationships, and particularly serodiscordant ones and how you can negotiate safe sex. We also have counselling services that help people who are experiencing domestic violence and drug and alcohol problems. All of these things impact on HIV prevention."
But it is ACON's general approach to giving honest, accurate, up-to-date information and the constant adaptation of campaign materials to specific target audiences that has kept the safe sex message strong, says Clayton. "If you go out into just about any gay bar in Sydney you're going to see campaign material from ACON and you're going to find condoms and lube readily available, creating an environment in which safe sex is seen as the norm.
"When we did have an increase in infections, quite a large increase in NSW in 2002 and 2003, we produced a lot of material which told people exactly what had changed, what was different, why we were seeing an increase. We targeted those who were more sexually active."
A consistent trend in the annual Sydney Gay Community Periodic Surveys is the increase in the use of the Internet to find sexual partners. As more traditional venues such as bars, clubs and beats lose popularity to the web, Clayton says innovation is necessary to get the safe sex message across in cyberspace.
"But if men are picking each other up off the internet and going to each others homes we don't have anything like that opportunity to provide information, or to make sure that condoms and lube are available. So we are looking desperately for much more innovative ways of getting that message across. We are going into partnership with the National Centre in HIV Social Research, which is doing research to provide us with the data we need to target programs on the Internet well.
"We're also going into joint programs with organisations like Gaydar, who are providing facilities for organisations such as ACON to provide health information over the Internet and in chat rooms."
The ACON Join Me in October! campaign that ran throughout October 2007 to encourage higher rates of testing and awareness for syphilis had an Internet component, says ACON community health director Nick Corrigan. "We set up a profile on www.sexpigs.com.au because it is popular with men who have group sex. We chatted with individuals and had some interesting conversations. This kind of thing generates a sense of looking after one another, sending the message that if you're looking after yourself, you're also looking after your community."
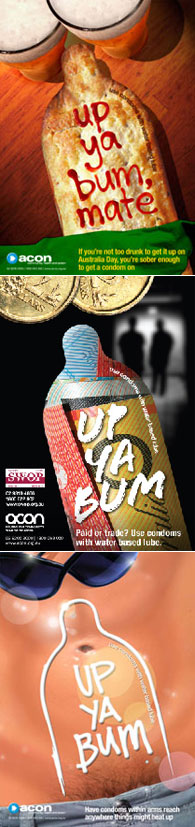
Other recent ACON campaigns have included Three or More, information for those planning home parties; Up Ya Bum, a poster campaign about condom use which includes sex workers in it's target audience, and the website www.whytest.org, where SMS messages can be sent via the website to inform recent sex partners, anonymously if desired, that they should get tested as the sender has had a positive test result for an STI.
While condoms and lube remain the focus for the majority of safe sex campaigns, the gay community are doing informal safe sex work of their own.
"When we look at increases or decreases in reporting of condom use, we have to remember the way the data is collected," says Clayton. "Gay men who report that they have on even one occasion in the last six months not used a condom for sex isn't wholesale stopping of using condoms. For the most part it's occasional non-use, and when not using condoms usually there are other risk reduction practices put in place.
"Two more common techniques are what is called strategic positioning by researchers, which entails being a bottom if you're positive and being a top if you're negative and trying that way to reduce transmission of HIV, and serosorting - where you choose, or try to choose your sexual partner based on their HIV status. The theory goes that if you're HIV negative and you only have sex with men who are HIV-, HIV won't be transmitted. Equally if you're HIV+ and your partner is too, you're not going to be passing on HIV."
"The flaw in all of this," says Clayton, "is if you're negative you can't tell that the other person is negative and the guy may have been negative in his last test but may have since his last test become HIV+. And certainly neither of these practices is going to protect you from STIs, so what we're seeing with those increases is guys who are looking for ways to have sex without a condom that won't be unsafe."
To this end an ACON serosorting campaign is being devised currently, says Corrigan. "The campaign is called You Just Don't Know and aims to tackle the presumptions that men make about each others HIV status. The other benefit of this campaign is that it will acknowledge how HIV+ men do take responsibility and care not to infect others."
At a time when HIV infection rates are rising in most large cities throughout the globe reports like the Swiss Federal AIDS Commission's January 2008 publication cause headaches for safe sex advocates. The report claimed that people with HIV do not risk transmitting the virus sexually provided they have had an undetectable viral load for at least six months, are adhering to a strict antiretroviral treatment, and do not have a sexually transmitted disease.
Clayton says this is essentially in line with ACON policy in that if you have an undetectable viral load the chances are you're pretty unlikely to pass on HIV. However, "the problem is your viral load can change rapidly so if you are sick and you're throwing up all the time you're probably not taking your medications in properly, then your viral load can move up rapidly. If you have an STI it will, and there is a really high rate of STIs in Sydney.
"It could be that you're changing treatment regimes, or for any number of reasons, your viral load can change rapidly, so it's not a replacement for safe sex. And the context for the Swiss commissioned statement was focused entirely on heterosexual couples that wanted to have children. They weren't suggesting that people should abandon condoms in favour of viral load monitoring for casual encounters. The report has been roundly criticised all around the globe."
