The Global Forum for MSM and HIV has released an analysis of its 2012 Global Men’s Health and Rights Study (GMHRS) concentrating on young men under 30 who have sex with men (MSM), complementing the full report which came out in December 2012.
Taken together, both reports reveal that MSM globally are faced with high levels of homophobia, stigma and discrimination, which are significantly associated with difficulties in accessing condoms and lubricant, HIV and STI testing, and HIV treatment.
The youth report also shows that, for most indicators, access to HIV and sexual health services, poverty and poor housing levels, and experience of homophobia and violence are worse for young MSM than for older ones.
One other and perhaps surprising set of findings were those testing respondents’ knowledge of and attitudes towards pre-exposure prophylaxis (PrEP). The more knowledgeable about PrEP and connected to the MSM community men were, and the higher the income of their country, the less likely they were to have positive attitudes towards PrEP; conversely, men who had experienced high levels of homophobia, violence and stigma from healthcare workers were more likely to be positive about PrEP.
For more, download report at Msmgf.org
The Global Men's Health and Rights Study
The study was conducted as an internet survey between April and August 2012; 5779 men accessed it and 4083 fully completed it. Fifty-eight per cent of men completed it in English with relatively high numbers of responses in Spanish, Chinese and Russian.
The quantitative internet survey was supplemented by qualitative work in Africa, in the shape of five focus groups containing a total of 71 men that met in community-based organisations in Kenya, Nigeria and South Africa. These added extra personal perspective and testimony to some of the findings.
Who answered the survey?
Most respondents described themselves as gay (84%) or bisexual (13%). Their average age was 35 but there was a huge age range, from 12 to 90, and a huge geographical range, with 165 countries represented.
Three-quarters of responses were from high- or upper-middle-income countries, 20% from low-middle-income countries, and only 4% from low-income countries (these are chiefly in Africa but also include countries such as Bangladesh and Haiti). Because of poor access to the internet in low-income countries, a paper-and-pencil version of the survey was also conducted in community settings in low-income countries; results from this have not yet been incorporated.
In terms of region, the best-represented was Asia with 28% of respondents, followed by North America and western Europe with 23%, eastern Europe and central Asia with 17%, Latin America with 15%, sub-Saharan Africa with 7%, and smaller representation from Oceania, the Caribbean and north Africa and the middle east. Young men under 30 were more likely to be Asian, east European or Latino, and less likely to come from North America or western Europe.
Eighteen per cent of respondents said they had HIV while another 17% were unsure. In the case of young men under 30, only 8% said they had HIV but 28% said they were unsure: given very high HIV infection rates in young men in some surveys, this may reflect lower testing rates rather than lower prevalence.
Eighty-two per cent of those in the general survey were on HIV treatment, but a lower proportion of young people (56%). This was reflected in the fact that they were much less likely to report that they were virally suppressed if they knew their viral load (38%, versus 73% for all HIV-positive respondents), were much more likely not to know their viral load anyway (33 versus 10%), and were more likely to have a CD4 count under 500 cells/mm3 (66 versus 55%).
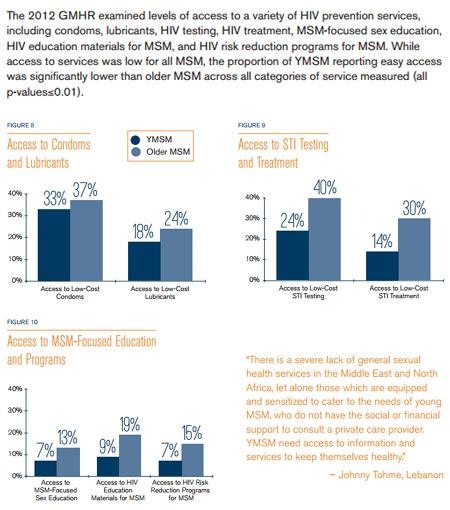
Access to HIV resources
Access to HIV services was conceptualised by being split into access to four basic needs: condoms, lubricants, testing and, for those with HIV, treatment. These were then related to country income level: low, lower-middle, upper-middle and high income. (To give examples of countries from the four categories, one can compare neighbours such as Cambodia (low income), Indonesia (lower-middle), Thailand (upper-middle) and Singapore (high income).
Participants rated access to HIV services on a five-point scale with five meaning “always accessible” and 1 meaning “never accessible”. It’s important to note that the study report only lists the proportion of people who answered with five points, so excludes “generally but not always accessible”.
With that caveat in mind, the report shows that in no income stratum were condoms and lubricants classed as ‘easily accessible’ by a majority. About 45% of high-income respondents and only a third in the other categories said condoms were easily accessible (overall average, 37%) and about a third of high-income respondents said lubes were easily accessible, only a quarter overall, and in low-income countries, only 8% said they were easily accessible.
In the case of HIV testing, where overall 40% said they had easy access, there was an interesting split: there, access was lowest in the middle-income countries, where only a quarter said they had easy access to testing. It was significantly higher in low-income countries, where a third said they had easy access to HIV tests, and higher still in high-income countries, where over a half did. This may indicate that testing programmes in lower-income countries are meeting some success, or simply that many low-income countries have higher HIV prevalence, so more people test.
In terms of HIV treatment, about half of the HIV-positive men in high-income countries said they had easy access to it but only one in seven in low-income countries; globally, the average was 30%, but only 14% in young men under 30 (who may need it less if they have acquired HIV more recently).
The study also looked at access to educational programmes and material and found that only 14% of men had access to MSM-focused sex education and HIV risk-reduction programmes, and only 19% to HIV education materials.
In all cases, young people under had poorer access to HIV resources but especially to HIV testing, where only 24% said they had easy access compared to 40% of respondents in general.
Structural barriers to HIV resources
The study analysed how social attitudes and phenomena affected access to HIV prevention and treatment. In multivariate analysis, there was a strong and independent relationship between respondent’s perception that people in their country were strongly homophobic, and poor access to condoms, lubes, testing and treatment. Perceived provider stigma also independently impacted on the availability of condoms.
Conversely, being ‘engaged with the community’ – which generally meant some kind of involvement in an MSM or HIV support group – and even more so, knowing a trusted healthcare provider, were independently associated with better access.
However, the study also uncovered a paradox. It found that ‘outness’ – the degree to which respondents said they were publicly gay – was associated with lower access to lubes and having experienced negative consequences to being ‘out’ with lower access to testing. This is underlined by some individual comments from the focus groups: one speaker said “We must teach young men who come from country to behave like ‘real men’ when they are out in public. Otherwise, they will get beaten up." While this and similar comments may betray some internalised homophobia, it may also recognise that in strongly homophobic cultures where gay men are stereotyped (and may stereotype themselves) as feminine, the only way to keep safe in public is to ‘pass as straight’.
Attitudes towards PrEP
In the internet survey, 48% of respondents indicated high knowledge of PrEP, and 23% middle knowledge, but there was very low awareness among the African focus groups.
Attitudes towards PrEP showed a consistent but surprising pattern. Generally low country income, homophobia, provider stigma, and violence and negative consequences after coming out were all associated with positive attitudes towards PrEP; conversely, high country income, being out as gay and being engaged with the gay community, and having a trusted provider, were associated with negative attitudes.
This is not the first survey to find a link between relative deprivation and acceptability of PrEP. Lower education level, for instance, and lower knowledge of PrEP, has been linked both with PrEP use and willingness to use it, as has more risk behaviour and higher vulnerability to HIV. More research will be needed to discover the reasons for this: are men with more education and more awareness of PrEP also more aware of its pitfalls or, conversely, are men who have particular difficulty accessing other HIV prevention methods seeing PrEP as a possible solution to their vulnerability to HIV infection?
Findings from the African focus groups
In the focus groups, several themes came through particularly strongly. One was that the most frequently cited negative consequence of homophobia and the criminalisation of sex between men is not violence, but blackmail and extortion: a large number of men mentioned having to pay blackmailers or having to pay extortionate rent, sometimes to other MSM, as the price for being allowed to live free from violence or legal persecution.
“I was kicked out of my apartment and it turned out it was another MSM who reported it,” said one. “He had to do it, or something bad would have happened to him.”
Another was that MSM globally spoke of high levels of depression and anxiety, some regarding it as an inevitable consequence of their sexuality. “Most of us have high levels of depression,” said one. “We learn to live with it or die.”
A third was the frequent experience of negative attitudes by healthcare staff: one said: “I went to the hospital and the nurse pulled out a Bible to lecture me about being gay. She did not pay attention to my health.” Another said: “The doctor brought in other doctors to see ‘The gay man’, as if I was a spectacle for show. I will not go back.”
A final one, looking on the more positive side, was that a stable job and/or a community-based organisation (CBO) that offered a safe space were both positively associated with better access to health services. The latter was especially important for young gay men under 30, who were ten times more likely to report having no income than men over 30. “Even if it is in secret,” said one discussant, “in our CBO we have a sense of community. We can support and learn from each other.”
Even there, though, there was worry and paranoia about being ‘outed’: “There is a lot of gossip among us that is sometimes good,” said one, “but it would be good to feel my business will not be out in the street.”
This article was first published by NAM/Aidsmap.com and is republished with permission.
References
The Global Forum for MSM and HIV. Access to HIV Prevention and Treatment for Men Who Have Sex with Men: Findings from the 2012 Global Men‘s Health and Rights Study (GMHR). 2012.
The Global Forum for MSM and HIV. Young Men Who Have Sex with Men: Health,access, & HIV. Data from the 2012 Global Men‘s Health & Rights (GMHR) Survey. 2013.








 列印版本
列印版本

















讀者回應
搶先發表第一個回應吧!
請先登入再使用此功能。